|

Laser Eye Surgery...
The intent of
(refractive) eye
surgery is to change the natural curvature of the cornea in order to alter the eye's focusing
power. There are
two main surgical techniques in the eye surgeon's arsenal to accomplish this goal:
PRK (Photo Refractive Keratectomy), and LASIK (Laser Assisted In-situ
Kerato-mileusis). LTK (Laser thermal keratoplasty) is a relatively new
application of laser technology and hyperopic
radiofrequency thermo-keratoplasty in in the testing stage.
Both PRK and LASIK
begin with the application of topical anesthesia to the eyeball. These eye drops numb the cornea to any
sensation. Once the cornea is sufficiently numb, the lids are then retracted and the cornea is marked with a special ink. This is to delineate the diameter of a clear zone directly in front of the pupil.
Use of the Excimer Laser
In the early 80s, eye surgeons became aware of the Excimer laser. While most surgical laser beams affect tissue by producing heat, the Excimer laser uses a charged mixture of argon and fluorine gases to produce a cool beam of ultraviolet light. The beam breaks the molecular bonds between cells and vaporizes tissue, one microscopic layer at a time. The Excimer laser was formally approved for use in PRK in 1995.
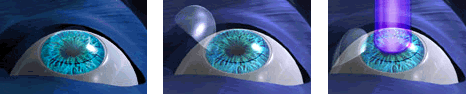
  Photo Refractive Keratectomy (PRK)
uses the Excimer laser to reshape the cornea in an effort to
change the refractive characteristics of the eye and thereby correct or lessen
vision problems. Before the laser is applied, the epithelial (outer) layer of the cornea is removed by either mechanical
or chemical means. The laser is then used to vaporize several microns of tissue from the central and mid
cornea. The epithelium usually regrows over the treated area within several days. To reduce the amount of myopia in the eye, the cornea is flattened by removing more tissue from the center of the cornea than from the midzone cornea. The resultant central corneal flattening moves the focus point farther back toward its desired spot on the retina. To reduce hyperopia, more tissue is removed from the midzone cornea, thereby steepening the central cornea.
Photo Refractive Keratectomy (PRK)
uses the Excimer laser to reshape the cornea in an effort to
change the refractive characteristics of the eye and thereby correct or lessen
vision problems. Before the laser is applied, the epithelial (outer) layer of the cornea is removed by either mechanical
or chemical means. The laser is then used to vaporize several microns of tissue from the central and mid
cornea. The epithelium usually regrows over the treated area within several days. To reduce the amount of myopia in the eye, the cornea is flattened by removing more tissue from the center of the cornea than from the midzone cornea. The resultant central corneal flattening moves the focus point farther back toward its desired spot on the retina. To reduce hyperopia, more tissue is removed from the midzone cornea, thereby steepening the central cornea.
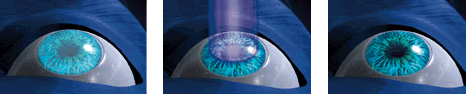
  Laser Assisted In-situ Keratomileusis (LASIK) is similar to PRK,
but does not treat or alter the very front surface of the cornea. In the LASIK procedure, a liquid anesthetic is dropped into the patient's eye, numbing it for surgery. The surgeon then props the eyelids open and marks the cornea with water soluble ink to guide in the later repositioning of the flap. A suction ring is placed on the eye to secure the eye and maintain pressure within the eye while the cornea is drawn outward.
Simultaneously, a microkeratome (a small, automated scalpel) is placed in the track of the suction ring. The blade of the microkeratome then moves across the cornea, creating a flap of corneal tissue some 30-40%
deep into the total corneal thickness. This layer is not cut away completely, but remains attached at one side and is then opened like a door on a hinge to reveal the stromal bed beneath.
Laser Assisted In-situ Keratomileusis (LASIK) is similar to PRK,
but does not treat or alter the very front surface of the cornea. In the LASIK procedure, a liquid anesthetic is dropped into the patient's eye, numbing it for surgery. The surgeon then props the eyelids open and marks the cornea with water soluble ink to guide in the later repositioning of the flap. A suction ring is placed on the eye to secure the eye and maintain pressure within the eye while the cornea is drawn outward.
Simultaneously, a microkeratome (a small, automated scalpel) is placed in the track of the suction ring. The blade of the microkeratome then moves across the cornea, creating a flap of corneal tissue some 30-40%
deep into the total corneal thickness. This layer is not cut away completely, but remains attached at one side and is then opened like a door on a hinge to reveal the stromal bed beneath.
Once the upper corneal flap has been folded back, the Excimer laser is then employed to vaporize the amount of underlying corneal tissue believed necessary to reshape the corneal curvature to the desired degree. To correct myopia, the laser trims the cornea's center, making it flatter. For hyperopia, a
doughnut shaped ring of tissue is removed. The laser is programmed to ablate the necessary amount with a modified version of the patient's glasses or contact lens prescription. The corneal flap is then repositioned to its original position on the stromal bed where it
should adhere over the next several months.
  IntraLase FS Laser and
IntraLASIK. IntraLASIK is a variation of LASIK using the IntraLase
FS femtosecond laser instead of a microkeratome blade to cut the
corneal flap. As in regular LASIK, an excimer laser then shapes the
underlying corneal tissue.
IntraLase FS Laser and
IntraLASIK. IntraLASIK is a variation of LASIK using the IntraLase
FS femtosecond laser instead of a microkeratome blade to cut the
corneal flap. As in regular LASIK, an excimer laser then shapes the
underlying corneal tissue.
IntraLase announced the placement of 22 systems during 2Q03, bringing
total placement to 64. No severe complications have been recorded in
69,000 IntraLASIK procedures in the U.S., an improvement over
traditional microkeratome procedures, which claim to have a 1% to 3%
incidence of complications.
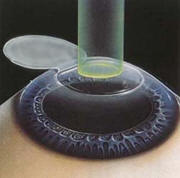
  Laser Thermal Keratoplasty (LTK) uses the holmium YAG
laser to heat the tissue of the cornea, causing it to
shrink and steepen the front of the eye to change the focus of
incoming light onto the retina, the light-sensitive layer of tissue
at the back of the eye. The goal of LTK is to improve the
patient’s ability to see objects at a distance. It is unsure how
long LTK results will last. When the US Food and Drug Administration
approved LTK in the summer of 2000, it was originally labeled a
“temporary” treatment. But some studies indicate could work
longer than initially believed and the FDA has removed the word
temporary. The laser device was approved to be used to treat
patients who have farsightedness (between +0.75 to +2.5 diopters ),
who are at least 40 years of age, and whose visual acuity has
changed very little over time (that is, the patient’s glasses
prescription has changed no more than 0.50 diopter in the previous
six months.)
Laser Thermal Keratoplasty (LTK) uses the holmium YAG
laser to heat the tissue of the cornea, causing it to
shrink and steepen the front of the eye to change the focus of
incoming light onto the retina, the light-sensitive layer of tissue
at the back of the eye. The goal of LTK is to improve the
patient’s ability to see objects at a distance. It is unsure how
long LTK results will last. When the US Food and Drug Administration
approved LTK in the summer of 2000, it was originally labeled a
“temporary” treatment. But some studies indicate could work
longer than initially believed and the FDA has removed the word
temporary. The laser device was approved to be used to treat
patients who have farsightedness (between +0.75 to +2.5 diopters ),
who are at least 40 years of age, and whose visual acuity has
changed very little over time (that is, the patient’s glasses
prescription has changed no more than 0.50 diopter in the previous
six months.)
According
to the FDA, this treatment may improve distance vision in
far-sighted people who have difficulty seeing clearly at a distance.
Although some patients may retain some or all of the correction
achieved during the surgery, for most people the amount of
farsightedness correction achieved will decrease over time. The
amount of correction remaining at 24 months is typically about half
of the correction observed at 6 months. Some patients will regress
completely. How long any significant portion of the correction lasts
depends on the amount of correction attempted and age.
  Laser Epithelial Keratomileusis (LASEK). This new procedure resembles LASIK but
still has significant differences. In the LASEK surgery the surgeon
cuts an ultra-thin flap of the outermost part of the cornea, the
epithelium and applies an alcohol solution to loosen it up and make
it easily manipulable. It must be noted that there are serious
questions as to the impact this alcohol has as it permeates various
structures in the eye.
Laser Epithelial Keratomileusis (LASEK). This new procedure resembles LASIK but
still has significant differences. In the LASEK surgery the surgeon
cuts an ultra-thin flap of the outermost part of the cornea, the
epithelium and applies an alcohol solution to loosen it up and make
it easily manipulable. It must be noted that there are serious
questions as to the impact this alcohol has as it permeates various
structures in the eye.
The surgeon then lifts the flap he has just
created and then uses the same laser used in a LASIK procedure to
ablate (vaporize) the corneal tissue at a layer closer to the
outer surface than the way it's done in LASIK. The
epithelial flap is then replaced and the patient is given a contact
lens to wear for a few days as the eye heals.
The procedure is in clinical trials. Some
think LASEK may turn out to be an alternative to LASIK for those
with low to moderate myopia. It has also been tested for those with
hyperopia. LASEK is being considered as an alternative to LASIK
because it may eliminate some of the flap related complication
currently experienced in LASIK.
There are other, experimental, procedures
currently undergoing clinical trials:
 Laser Thermal Keratoplasty (LTK),Collagen
in the cornea is heated with laser beams to correct hyperopia, or
farsightedness. Laser Thermal Keratoplasty (LTK),Collagen
in the cornea is heated with laser beams to correct hyperopia, or
farsightedness.
 Radio frequency keratoplasty - Similar to LTK, but radio waves
rather than laser energy are used to heat collagen in the cornea.
Radio frequency keratoplasty - Similar to LTK, but radio waves
rather than laser energy are used to heat collagen in the cornea.
 Epi-LASIK - In Epi-LASIK, a blunt keratome
(different from the blade in conventional LASIK) creates a thin sheet from
the surface of the eye (the epithelium), rather than a deeper
blade-produced cut, as
Epi-LASIK - In Epi-LASIK, a blunt keratome
(different from the blade in conventional LASIK) creates a thin sheet from
the surface of the eye (the epithelium), rather than a deeper
blade-produced cut, as
 in LASIK. Displacing the epithelium makes
this procedure similar to LASEK or PRK, but the blunt keratome
obviates the need for cell-toxic alcohol, used in those two
procedures. Since the epithelium is still bound via the flap,
there's a better chance of survival of the epithelial cells, and
possibly similar post-procedure comfort and vision to LASIK.Epi-Lasik
is intended to preserve the structural integrity of the stroma and
is expected to minimize discomfort, shorten the length of visual
recovery, and reduce the incidence of haze associated with other
surface ablation procedures, such as PRK and LASEK in LASIK. Displacing the epithelium makes
this procedure similar to LASEK or PRK, but the blunt keratome
obviates the need for cell-toxic alcohol, used in those two
procedures. Since the epithelium is still bound via the flap,
there's a better chance of survival of the epithelial cells, and
possibly similar post-procedure comfort and vision to LASIK.Epi-Lasik
is intended to preserve the structural integrity of the stroma and
is expected to minimize discomfort, shorten the length of visual
recovery, and reduce the incidence of haze associated with other
surface ablation procedures, such as PRK and LASEK
 Advanced Surface Ablation
(ASA) - Advanced
Surface Ablation is sometimes referred to as blade-Free correction. ASA is a
form of photorefractive keratectomy (PRK) that uses excimer lasers capable of
eye tracking and wavefront customized treatment to reshape the front surface of
the cornea to correct vision. There is no flap made in ASA surgery. A temporary
or 'bandage' soft contact lens is placed on the eye for a few days following
surgery to assist in the healing process.
Advanced Surface Ablation
(ASA) - Advanced
Surface Ablation is sometimes referred to as blade-Free correction. ASA is a
form of photorefractive keratectomy (PRK) that uses excimer lasers capable of
eye tracking and wavefront customized treatment to reshape the front surface of
the cornea to correct vision. There is no flap made in ASA surgery. A temporary
or 'bandage' soft contact lens is placed on the eye for a few days following
surgery to assist in the healing process.
| 